

Articles
How To Store Insulin
Modified: January 6, 2024
Learn the best practices for storing insulin and keeping it safe. Read our informative articles on proper storage techniques and maintaining insulin potency.
(Many of the links in this article redirect to a specific reviewed product. Your purchase of these products through affiliate links helps to generate commission for Storables.com, at no extra cost. Learn more)
Introduction
Insulin is a life-saving medication for individuals with diabetes. It helps to regulate blood sugar levels and keeps the body functioning properly. But proper insulin storage is crucial to maintain its effectiveness.
Improper storage can lead to the loss of potency of insulin, rendering it ineffective in managing blood sugar levels. Factors such as temperature, light, and duration can significantly impact insulin stability. Therefore, it is essential to understand the right storage conditions to ensure the safety and efficacy of this vital medication.
In this article, we will delve into the details of insulin storage, including guidelines for refrigeration and room temperature storage, protecting insulin from extreme temperatures and light, differences between insulin vials and pens, and essential tips for proper insulin storage. Whether you are a diabetic patient or a caregiver, this guide will provide you with valuable insights to help you store insulin effectively.
Key Takeaways:
- Proper insulin storage is crucial for maintaining its effectiveness. Refrigeration and room temperature storage, avoiding extreme temperatures and light exposure, and understanding insulin types are key factors to consider.
- When traveling with insulin, careful planning is essential. Carry extra supplies, keep insulin cool, be aware of local regulations, and monitor insulin quality to ensure its safety and efficacy during your journey.
Understanding Insulin
Insulin is a hormone produced by the pancreas that plays a crucial role in regulating blood sugar levels. For individuals with diabetes, their bodies either do not produce enough insulin or are unable to effectively use the insulin produced. As a result, they need to take insulin through injections or an insulin pump to manage their blood sugar levels.
Insulin comes in different forms, including vials and pens, and there are various types of insulin available, such as rapid-acting, short-acting, intermediate-acting, and long-acting insulin. Each type has its own specific characteristics and is used to manage blood sugar levels in different ways.
Rapid-acting insulin starts working within minutes and lasts for a few hours. It is typically taken around mealtime to manage the rise in blood sugar levels after eating. Short-acting insulin takes effect within half an hour and lasts for a few hours. It is commonly used before meals to help control blood sugar spikes.
Intermediate-acting insulin has a slower onset and lasts longer, typically used to cover the body’s insulin needs between meals and overnight. Long-acting insulin has a slow and steady release, providing a baseline insulin level throughout the day and night.
It is crucial to note that different types of insulin have specific storage requirements. Understanding the type of insulin you are using is vital for proper storage and maintenance of its potency.
Proper Storage Conditions
Proper storage conditions play a vital role in maintaining the potency and effectiveness of insulin. Factors such as temperature, light, and duration can significantly impact the stability of insulin. Here are some key points to consider:
Refrigeration
Refrigeration is the most common way to store insulin. Insulin should be stored in the refrigerator between 36°F and 46°F (2°C and 8°C). It is essential to keep insulin away from the back of the refrigerator, as extreme cold temperatures near the freezer can affect its effectiveness.
Insulin should not be frozen. Freezing can cause insulin to break down, making it ineffective. If insulin accidentally freezes, it should be discarded, as its potency cannot be guaranteed.
Room Temperature Storage
Some types of insulin, such as rapid-acting and short-acting insulin, can be stored at room temperature for a limited period. The recommended temperature range for room temperature storage is typically between 59°F and 86°F (15°C and 30°C).
It is important to check the specific recommendations provided by the insulin manufacturer, as some types of insulin have shorter room temperature storage durations than others. Keeping insulin in a cool, dry place can help maintain its stability during room temperature storage.
Read more: How To Store Store-Bought Bread
Avoiding Extreme Temperatures
Extreme temperatures, both hot and cold, can affect the efficacy of insulin. It is crucial to avoid exposing insulin to temperatures above 86°F (30°C) or below 36°F (2°C).
Extreme heat can cause insulin to break down, lose its effectiveness, and become less potent. Similarly, extreme cold can cause insulin to freeze and become ineffective. Avoid storing insulin near direct sources of heat, such as radiators or vents, and refrain from leaving insulin in a hot car.
Protecting from Light
Insulin should be protected from direct light, including sunlight and artificial light sources. Exposure to light can cause insulin degradation and result in decreased potency.
Keep insulin stored in its original packaging or use opaque containers to shield it from light. If you need to transport insulin, consider using a dedicated insulin travel case or wrap it in aluminum foil to provide additional protection.
Proper disposal of insulin is equally important. Expired or damaged insulin should be discarded as per your local guidelines for the safe disposal of medical waste.
By following these proper storage conditions, you can ensure the longevity and effectiveness of your insulin supply, helping to manage your diabetes effectively.
Refrigeration
Refrigeration is one of the most common methods of storing insulin. It helps to maintain the stability and potency of the medication. Here are some important considerations when it comes to refrigerating insulin:
- Temperature: Insulin should be stored in the refrigerator at a temperature range of 36°F to 46°F (2°C to 8°C). This helps to maintain the chemical structure of the insulin and ensures its effectiveness.
- Placement: It is advisable to store insulin away from the back of the refrigerator, as this area tends to be colder due to its proximity to the freezer. Placing insulin in the main compartment, away from the freezer and cooling elements, will help maintain a consistent temperature.
- Container: Insulin vials or pens should always be stored in their original packaging or in a designated insulin storage container. This helps to protect the medication from exposure to light and potential damage.
- Avoid Freezing: Insulin should never be frozen. Freezing can cause denaturation and breakdown of the medication, rendering it ineffective. If insulin accidentally freezes, it should be discarded, as its potency cannot be guaranteed.
- Expiration Dates: Always check the expiration dates of your insulin supplies. Expired insulin should be discarded, as it may have reduced effectiveness in managing blood sugar levels.
It is important to note that insulin stored in the refrigerator may develop small crystals or clumps. Insulin should be gently mixed or rolled between your hands to redistribute suspended particles before each use. However, never shake the insulin vigorously, as it may affect its effectiveness.
When traveling or during power outages, it’s essential to keep insulin at the correct temperature. Insulated travel cases or cooling wallets can help maintain the appropriate temperature during short trips. If refrigeration is unavailable for an extended period, it is advisable to use alternative storage methods, such as cooling packs specifically designed for insulin storage.
By adhering to proper refrigeration practices, you can ensure the integrity of your insulin and maximize its effectiveness in managing your diabetes.
Room Temperature Storage
While refrigeration is the recommended method for storing insulin, some types of insulin can be safely stored at room temperature for a certain period. Here is some important information about room temperature storage of insulin:
- Temperature Range: The recommended temperature range for room temperature storage of insulin is typically between 59°F and 86°F (15°C and 30°C). Keeping insulin within this range helps maintain its effectiveness.
- Duration: Each type of insulin has a specific allowable duration for room temperature storage. Rapid-acting and short-acting insulin, for example, can typically be kept at room temperature for up to 28 days. However, it is important to check the specific storage guidelines provided by the insulin manufacturer.
- Checking Expiration Dates: Make sure to regularly check the expiration dates of your insulin supplies. Expired insulin should never be used, regardless of the storage method.
- Insulin Stability: Insulin stored at room temperature may experience slight changes in stability compared to refrigerated insulin. Factors such as humidity, exposure to light, and fluctuating temperatures can impact insulin potency. Therefore, it is essential to monitor the temperature and conditions of the storage area.
- Dry and Cool Place: When storing insulin at room temperature, ensure it is kept in a cool, dry place away from direct sunlight and heat sources. Avoid storing insulin near windowsills, radiators, or other areas where temperature fluctuations are likely to occur.
It is important to note that once insulin is taken out of the refrigerator and stored at room temperature, it should not be returned to the refrigerator. Doing so can affect the stability and effectiveness of the insulin.
If the recommended duration for room temperature storage expires and there is still insulin remaining, it should be discarded. It is better to prioritize safety and efficacy rather than using insulin that may have lost its potency.
Always consult with your healthcare provider or pharmacist if you have any questions or concerns regarding the storage of your specific type of insulin.
By following the recommended guidelines for room temperature storage, you can ensure that your insulin remains safe and effective for the prescribed duration.
Read more: How To Store Basil From Grocery Store
Avoiding Extreme Temperatures
Extreme temperatures, both hot and cold, can have a detrimental effect on the potency and effectiveness of insulin. It is crucial to protect insulin from extreme temperatures to ensure its stability. Here are some key points to consider:
- High Temperatures: Insulin should be kept away from temperatures above 86°F (30°C). Excessive heat can cause insulin to break down, potentially rendering it ineffective. Avoid leaving insulin in hot environments such as parked cars, direct sunlight, or near heat sources like radiators.
- Cold Temperatures: Insulin is also susceptible to the damaging effects of extreme cold. It should never be exposed to temperatures below 36°F (2°C). Freezing can cause the breakdown of insulin, leading to a loss of effectiveness. Be cautious when storing insulin in unheated areas during the winter season.
- Traveling: When traveling, ensure you have a proper plan to protect your insulin from extreme temperatures. Consider using an insulated travel case or a cooling wallet designed for insulin storage. These can help maintain the required temperature while on the go.
- Power Outages: During power outages, it is crucial to have a backup plan to safeguard your insulin. If refrigeration is unavailable for an extended period, consider using portable refrigeration options such as coolers or cooling packs specifically designed for insulin storage. These can help maintain the required temperature for a certain duration.
- Monitoring: Regularly monitor the storage conditions and temperature of your insulin. Use a thermometer to check the temperature in the storage area and ensure it remains within the safe range. If you suspect that insulin has been exposed to extreme temperatures, it is advisable to consult with your healthcare provider or pharmacist for guidance.
Remember that once insulin has been exposed to extreme temperatures, its effectiveness may be compromised. If you have any doubts about the potency or stability of your insulin, it is always better to err on the side of caution and consult with a healthcare professional.
By taking proper precautions and being proactive in avoiding extreme temperatures, you can help ensure that your insulin remains safe, effective, and capable of managing your diabetes effectively.
Protecting from Light
Protecting insulin from light is crucial to maintain its stability and effectiveness. Exposure to direct light, whether it is sunlight or artificial light sources, can lead to degradation of insulin molecules. Here are some important points to consider when it comes to protecting insulin from light:
- Original Packaging: Insulin should be stored in its original packaging until ready for use. The packaging is designed to provide protection from light, ensuring the stability of insulin. Avoid removing insulin from its original packaging until it is time for administration.
- Opaque Containers: If you need to transfer insulin to a different container, make sure to use a container that is opaque and light-resistant. This will prevent unnecessary exposure to light and help maintain insulin integrity.
- Travel Cases: When traveling, consider using a dedicated insulin travel case. These cases are designed to protect insulin from various factors, including light exposure. They provide an additional layer of protection during transit or while on the move.
- Aluminum Foil: If you do not have a specific insulin travel case and need to transport insulin, you can wrap the insulin vials or pens with aluminum foil. Aluminum foil acts as a barrier to light, providing temporary protection until the insulin can be stored appropriately.
- Storage Location: Choose a storage location for insulin that is away from direct sunlight and any other light sources. Avoid storing insulin near windows, light bulbs, or areas where it may be exposed to excessive light during the day.
Remember that even brief exposure to light over time can impact the stability of insulin. Therefore, it is important to be mindful of the storage conditions and take precautions to protect insulin from light.
Additionally, it is important to check the expiration dates of your insulin supplies regularly. Expired insulin should be discarded as per your local guidelines for the safe disposal of medical waste.
By following these guidelines and proper storage practices, you can help preserve the potency and effectiveness of your insulin, ensuring its reliability in managing your diabetes.
Insulin Vials vs. Insulin Pens
When it comes to administering insulin, there are two common options available: insulin vials and insulin pens. Each method has its own advantages and considerations. Let’s take a closer look at the differences between insulin vials and insulin pens:
Insulin Vials:
Insulin vials are small glass containers that contain a specific amount of insulin. They are typically used with a separate syringe for insulin administration. Here are some key points about insulin vials:
- Dosing Flexibility: Insulin vials allow for more flexibility in dosing as you can draw up different amounts of insulin as needed. This can be particularly beneficial for individuals who require specific insulin doses.
- Multiple Types of Insulin: Insulin vials accommodate various types of insulin, including rapid-acting, short-acting, intermediate-acting, and long-acting insulin, providing options to meet individual needs.
- Need for Syringe: Using insulin vials requires the use of a separate insulin syringe for administration. This may require extra steps for drawing up the correct insulin dose.
- Visibility of Insulin Amount: With insulin vials, the amount of insulin remaining can be easily seen, helping you keep track of your supply and plan for refills.
Read more: How To Store Arrows
Insulin Pens:
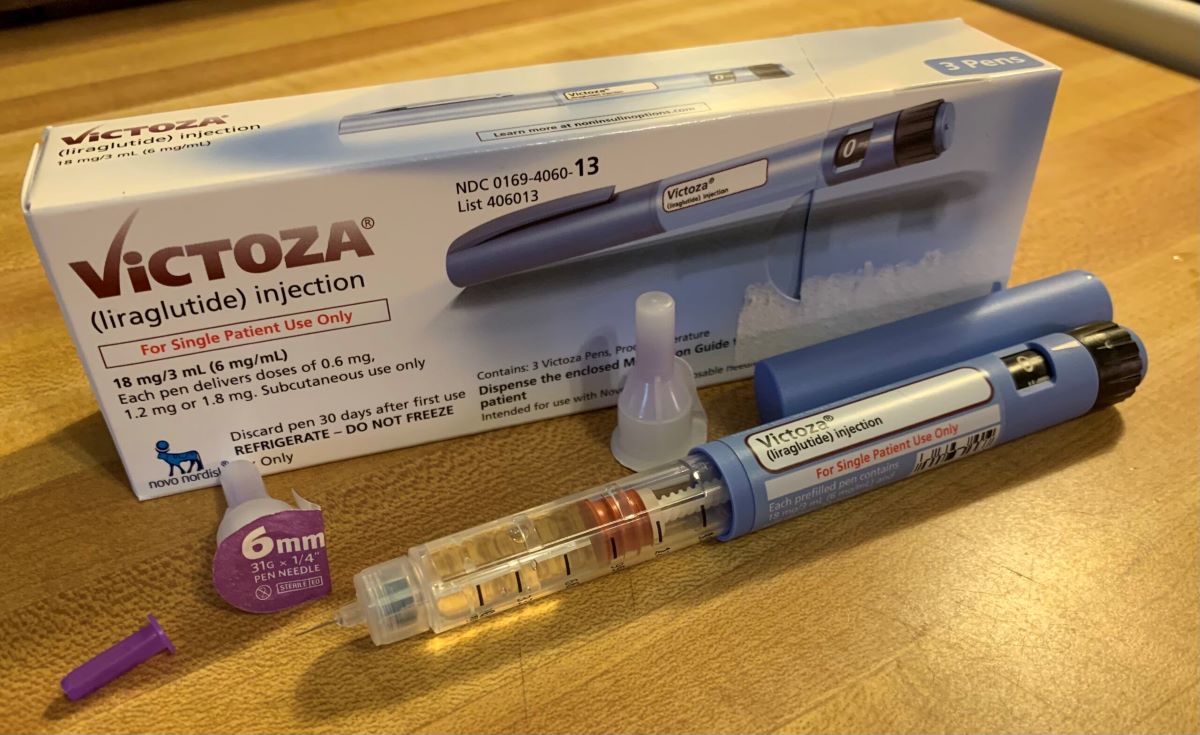
Insulin pens are pre-filled devices that contain a cartridge of insulin. They are designed with a built-in needle or a replaceable disposable needle. Here are some key points about insulin pens:
- Convenience and Portability: Insulin pens offer convenience, as they are pre-filled and ready for use. They are compact and easy to carry, making them ideal for individuals who need insulin injections on the go.
- Ease of Use: Insulin pens are user-friendly and do not require drawing up insulin doses with a syringe. They typically have a dial or button mechanism for adjusting the dose, making it easier to administer insulin accurately.
- Dosing Accuracy: Insulin pens provide more precision in dosing, as they usually have marked dose increments that help ensure accurate insulin delivery.
- Discreetness: Insulin pens are generally more discreet to use in public settings compared to vials and syringes.
Ultimately, the choice between insulin vials and insulin pens depends on individual preference, lifestyle, and specific needs. Some people may find the flexibility of vials and syringes more suitable, while others may prefer the convenience and ease of use offered by insulin pens.
It is important to consult with your healthcare provider to determine which method is best for you. They can provide guidance based on your specific insulin requirements and lifestyle factors.
Insulin Storage Tips
Proper storage of insulin is crucial for maintaining its potency and effectiveness. Here are some essential tips to ensure the safe storage of your insulin:
- Follow Manufacturer’s Instructions: Read and understand the storage instructions provided by the insulin manufacturer. Different types of insulin may have specific storage requirements, so it is important to adhere to their guidelines.
- Check Expiration Dates: Insulin has an expiration date, and using expired insulin may lead to reduced effectiveness. Regularly check the expiration dates on your insulin supplies, and discard any that have expired.
- Avoid Extreme Temperatures: Insulin should be protected from extreme temperatures. Avoid exposing insulin to temperatures above 86°F (30°C) or below 36°F (2°C), as these can impact its potency. Keep insulin away from direct sunlight, heat sources, and freezing conditions.
- Keep Insulin in Original Packaging: Insulin should be stored in its original packaging until ready for use. The packaging is designed to provide protection and maintain the stability of the insulin. Avoid transferring insulin to different containers unless necessary.
- Store Insulin in a Cool Place: Insulin should be stored in a cool place, away from direct sunlight and heat sources. Aim for a temperature range of 36°F to 46°F (2°C to 8°C) in the refrigerator. If storing at room temperature, ensure it remains between 59°F and 86°F (15°C and 30°C).
- Protect from Light: Insulin is sensitive to light, so it should be protected from direct sunlight and artificial light sources. Store insulin in a dark and cool spot, or use an opaque container or an insulin travel case to shield it from light.
- Do Not Share Insulin: Insulin is a medication tailored to individual needs. Never share insulin with others, as it may not be the appropriate type or dosage for their specific condition.
- Check for Changes: Before each use, visually inspect the insulin for any changes in appearance. Check for discoloration, particles, or clumping. If you notice any abnormalities, it is best to discard the insulin and use a fresh supply.
Remember, always consult with your healthcare provider or pharmacist if you have any concerns or questions regarding the storage of your insulin. They can provide personalized guidance based on your specific insulin type and needs.
By following these tips and practicing proper insulin storage, you can ensure the potency and effectiveness of your insulin, allowing you to effectively manage your diabetes.
Store insulin in the refrigerator at a temperature between 36°F and 46°F (2°C and 8°C). Avoid freezing or exposing it to direct sunlight or high temperatures. Keep it away from heat sources and extreme cold.
Traveling with Insulin
Traveling with insulin requires careful planning to ensure its safety and efficacy throughout your journey. Whether you are heading out for a short trip or a longer vacation, here are some important tips to keep in mind:
- Consult with Your Healthcare Provider: Before traveling, consult with your healthcare provider to discuss your travel plans. They can provide specific recommendations based on your insulin needs, dosage, and travel destination.
- Carry Extra Supplies: It’s always a good idea to carry more insulin supplies than you anticipate needing. Accidents happen, and you may encounter unexpected delays, so having extra insulin on hand ensures you won’t run out during your trip.
- Keep Insulin Cool: Insulin is sensitive to temperature, so it is important to keep it cool while traveling. Consider using an insulated travel case or a cooling wallet specifically designed for insulin storage. These will help maintain the temperature within the acceptable range.
- Avoid Excessive Heat or Cold: Protect insulin from extreme temperatures, both hot and cold. Avoid leaving insulin in a hot car, exposing it to direct sunlight, or storing it in a freezing cold environment. Use cooling methods, such as cool packs or gel packs, to help regulate the temperature during transit.
- Separate Supplies: If you are traveling with multiple insulin supplies, like vials, syringes, or pens, consider packing them separately. This way, if one bag is lost or damaged, you’ll have backups available in another bag.
- Carry Prescriptions and Documentation: It’s always a good idea to carry your insulin prescription and a letter from your healthcare provider stating that you are a diabetic and require insulin. This documentation can be helpful if you have any issues at airport security or customs checkpoints.
- Research Local Regulations: If you are traveling internationally, familiarize yourself with the local regulations regarding the transportation and use of insulin. Different countries may have specific requirements or restrictions that you need to be aware of.
- Keep Insulin with You: Never pack your insulin in checked luggage. Always keep it with you in your carry-on bag or purse. This ensures that you have immediate access to your insulin supplies and that they are not subjected to extreme temperatures in the cargo hold.
- Monitor Insulin Quality: During your trip, keep an eye on the quality of your insulin. Inspect it regularly for any signs of change, such as clumps, discoloration, or particles. If you notice any abnormalities, it is better to err on the side of caution and use a fresh supply.
Remember to check with the relevant transportation authorities regarding guidelines for traveling with insulin, especially if you are flying. Rules and regulations may vary, so it’s important to be well-informed and prepared.
By following these tips and taking necessary precautions, you can travel confidently with your insulin, ensuring its efficacy and your ability to effectively manage your diabetes while on the go.
Conclusion
Proper storage of insulin is vital to ensure its potency and effectiveness in managing diabetes. By understanding and following the recommended guidelines, you can maintain the integrity of your insulin supply and maximize its efficiency. Here are the key points to take away:
Insulin storage requires attention to temperature, light, and duration. Refrigeration is the most common method, with the temperature range of 36°F to 46°F (2°C to 8°C) being ideal. Room temperature storage, between 59°F and 86°F (15°C and 30°C), is acceptable for certain types of insulin, but be aware of the expiration date and specific storage guidelines for your insulin.
Extreme temperatures should be avoided, as both heat and freezing can impact insulin effectiveness. Protect insulin from direct light, as exposure can lead to degradation. Insulin vials and insulin pens are common methods of administration, each with its own advantages and considerations.
When traveling with insulin, plan ahead and carry extra supplies, keeping insulin cool and avoiding extreme temperatures. Familiarize yourself with local regulations, carry necessary documentation, and separate your supplies in case of loss or damage. Always keep insulin with you in your carry-on bag and monitor its quality regularly.
By adhering to these storage guidelines and taking necessary precautions, you can ensure the potency and effectiveness of your insulin, allowing you to effectively manage your diabetes and maintain better overall health.
Remember, it is always important to consult with your healthcare provider or pharmacist for personalized advice and guidance regarding the storage and usage of your specific insulin. They can provide the most accurate information based on your individual needs and circumstances.
With proper insulin storage, you can confidently take control of your diabetes and continue living a healthy and active life.
Frequently Asked Questions about How To Store Insulin
Was this page helpful?
At Storables.com, we guarantee accurate and reliable information. Our content, validated by Expert Board Contributors, is crafted following stringent Editorial Policies. We're committed to providing you with well-researched, expert-backed insights for all your informational needs.












0 thoughts on “How To Store Insulin”