Home>Furniture & Design>Bathroom Accessories>When To Change Toothbrush After Strep


Bathroom Accessories
When To Change Toothbrush After Strep
Modified: February 26, 2024
Learn when to change your toothbrush after having strep throat and find the best bathroom accessories for maintaining oral hygiene. Keep your dental routine on track.
(Many of the links in this article redirect to a specific reviewed product. Your purchase of these products through affiliate links helps to generate commission for Storables.com, at no extra cost. Learn more)
Introduction
Maintaining good oral hygiene is essential for overall health, and a crucial aspect of this is ensuring that our toothbrushes are clean and effective. However, many people may not be aware of the potential risks associated with using a toothbrush after being diagnosed with strep throat. In this article, we will delve into the importance of understanding strep throat, the potential contamination of toothbrushes, the recommended time to change a toothbrush after having strep throat, and other precautions to consider. By gaining insight into these aspects, you can better safeguard your oral health and prevent the spread of infections within your household.
Key Takeaways:
- Change your toothbrush as soon as you start antibiotics for strep throat to prevent reinfection and protect others. It’s like giving your toothbrush a fresh start for a healthier mouth!
- Keep your hands clean, avoid close contact, and disinfect surfaces to stop the spread of strep bacteria. By taking these steps, you can help create a safe and healthy environment for everyone.
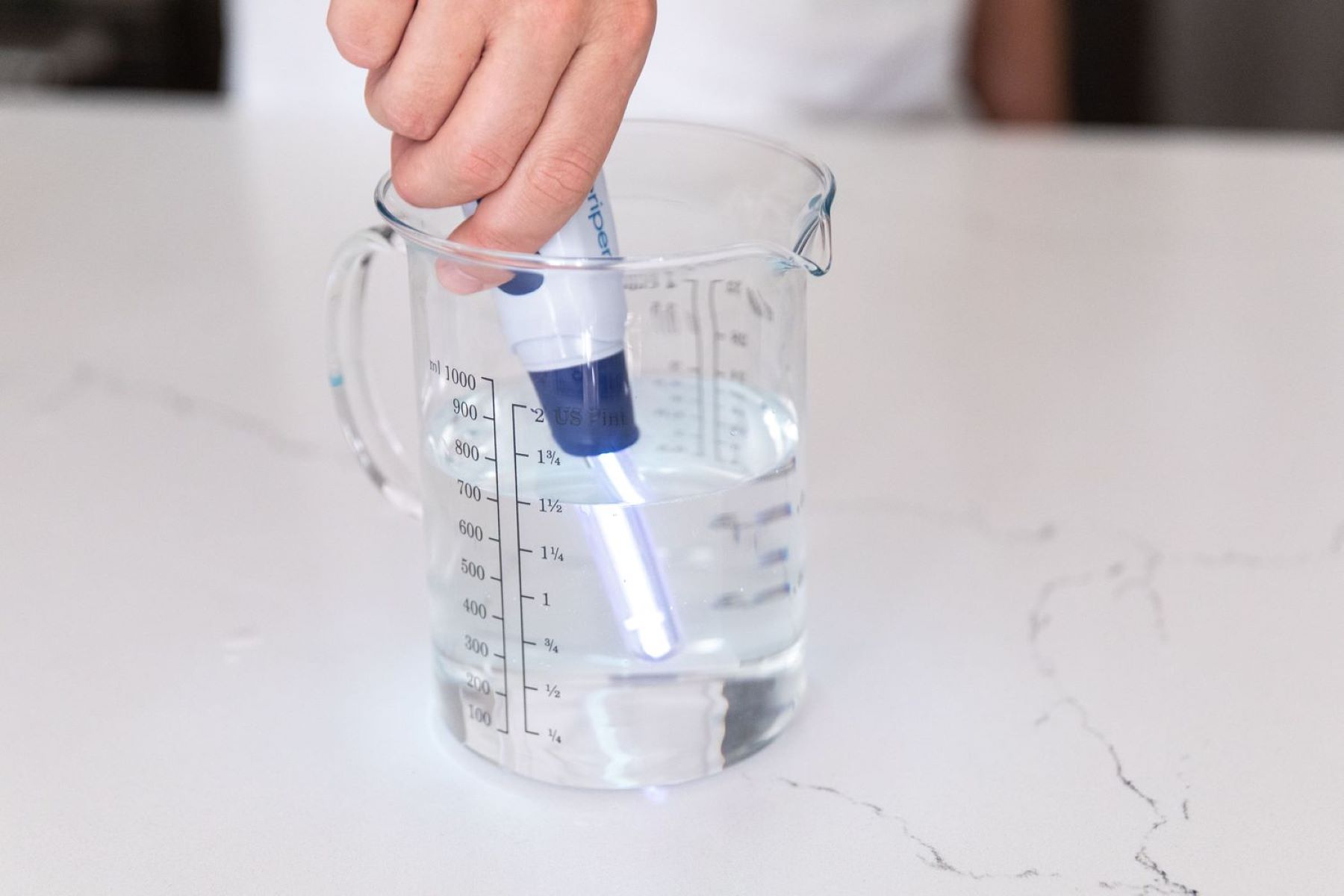
Read more: How To Disinfect Toothbrush After Strep
Understanding Strep Throat
Strep throat, also known as streptococcal pharyngitis, is a bacterial infection caused by Group A Streptococcus bacteria. This contagious condition commonly affects the throat and tonsils, leading to symptoms such as sore throat, difficulty swallowing, fever, and swollen lymph nodes. Strep throat is particularly prevalent among children and can spread rapidly in environments such as schools and daycare centers.
It is important to differentiate strep throat from other forms of sore throat, as the treatment and potential complications differ. Unlike viral infections, which can cause similar symptoms, strep throat requires specific antibiotic treatment to prevent complications such as rheumatic fever or kidney inflammation.
The diagnosis of strep throat is typically confirmed through a rapid strep test or throat culture conducted by a healthcare professional. If the test results are positive, prompt treatment with antibiotics is crucial to alleviate symptoms, reduce the duration of illness, and minimize the risk of spreading the infection to others.
Understanding the nature of strep throat is vital for implementing appropriate preventive measures, especially when it comes to personal hygiene practices and the management of household items such as toothbrushes. By being aware of the characteristics and potential consequences of strep throat, individuals can take proactive steps to protect themselves and their loved ones from the spread of this bacterial infection.
Contamination of Toothbrush
When an individual is diagnosed with strep throat, their toothbrush can become a potential reservoir for the bacteria. The act of brushing can introduce the streptococcal bacteria into the bristles and other parts of the toothbrush, leading to contamination. This poses a significant risk of reinfection or transmission of the bacteria to others sharing the same bathroom space.
The moist environment of the bathroom provides an ideal breeding ground for bacteria, including the streptococcal species. After each use, residual water and saliva on the toothbrush create a conducive environment for bacterial growth. Additionally, if the infected individual continues to use the same toothbrush during their illness, the bacteria can persist on the bristles, handle, and other surfaces of the toothbrush, increasing the likelihood of reinfection.
Furthermore, the simple act of flushing the toilet can aerosolize bacteria, potentially contaminating items in the immediate vicinity, including toothbrushes. This highlights the importance of proper toothbrush storage to minimize exposure to airborne bacteria.
It is crucial to recognize that the contamination of a toothbrush with streptococcal bacteria can perpetuate the cycle of infection within a household. Other family members or individuals sharing the same bathroom may inadvertently use the contaminated toothbrush, leading to the spread of the bacteria and subsequent cases of strep throat.
Understanding the potential contamination of toothbrushes in the context of strep throat underscores the importance of taking proactive measures to mitigate the risk of bacterial transmission. By addressing this aspect of personal hygiene, individuals can contribute to the overall prevention of recurrent infections and the spread of streptococcal bacteria within their living environment.
It is recommended to change your toothbrush after recovering from strep throat to prevent reinfection. Strep bacteria can survive on the bristles, so it’s best to start fresh.
Recommended Time to Change Toothbrush
After being diagnosed with strep throat, it is crucial to consider the appropriate time to change your toothbrush to prevent the risk of reinfection or transmission of the bacteria. The general consensus among healthcare professionals is to replace your toothbrush as soon as you start antibiotic treatment for strep throat. This proactive approach helps minimize the potential for the bacteria to linger on the toothbrush and reduces the risk of reinfection.
In most cases, the recommended time to change your toothbrush after strep throat is approximately 3 days after starting antibiotic therapy. This timeframe aligns with the typical course of antibiotic treatment for strep throat, which is usually 10 days. By replacing your toothbrush early in the treatment process, you can effectively eliminate the potential reservoir of streptococcal bacteria, reducing the likelihood of recurrent infection.
It is important to note that even after starting antibiotic treatment, individuals with strep throat remain contagious for the initial 24 to 48 hours until the antibiotics take effect. Therefore, changing the toothbrush promptly after beginning treatment is a proactive measure to prevent the spread of the bacteria to others and to minimize the risk of reinfection for the individual.
In situations where multiple family members share the same bathroom space, it is advisable for everyone to change their toothbrushes if one member is diagnosed with strep throat. This collective approach helps mitigate the risk of cross-contamination and supports a comprehensive effort to prevent the spread of the bacteria within the household.
Furthermore, it is essential to continue using the new toothbrush for a reasonable duration after completing the antibiotic course for strep throat. This practice ensures that any residual bacteria from the previous toothbrush are effectively eliminated, reducing the risk of reinfection or transmission.
By adhering to the recommended time frame for changing toothbrushes after strep throat, individuals can actively contribute to the containment of the bacteria and support the overall recovery process. This proactive measure aligns with the principles of effective personal hygiene and plays a pivotal role in preventing the recurrence and spread of streptococcal infections within the household.
Other Precautions to Take
In addition to changing the toothbrush after being diagnosed with strep throat, there are several other crucial precautions to consider in order to minimize the risk of bacterial transmission and support the recovery process. These measures encompass various aspects of personal hygiene and household management, aiming to create an environment that is conducive to preventing the spread of streptococcal bacteria.
-
Personal Hygiene Practices: Individuals with strep throat should practice thorough handwashing to reduce the likelihood of spreading the bacteria to surfaces, objects, or other individuals. Proper hand hygiene, including using soap and water or alcohol-based hand sanitizers, is essential, especially after coughing, sneezing, or touching the face. By maintaining diligent hand hygiene, individuals can minimize the risk of contaminating their surroundings and prevent the spread of the bacteria.
-
Isolation and Avoidance of Close Contact: During the contagious phase of strep throat, it is advisable to minimize close contact with others, particularly in crowded or confined spaces. This precaution helps reduce the risk of transmitting the bacteria to individuals who may be more susceptible to infection. Additionally, individuals with strep throat should consider temporary isolation within the household to prevent the spread of the bacteria to family members or housemates.
-
Disinfection of Common Surfaces: Regular cleaning and disinfection of commonly touched surfaces and objects in the household can contribute to the containment of streptococcal bacteria. This includes frequently used items such as doorknobs, light switches, faucets, and electronic devices. Using appropriate disinfectants and following recommended cleaning practices can help minimize the presence of the bacteria in the living environment, reducing the risk of recurrent infections.
-
Separation of Personal Items: In households where multiple individuals share the same bathroom, it is advisable to separate personal items such as toothbrushes, towels, and drinking glasses to prevent cross-contamination. This practice helps minimize the potential transfer of bacteria between individuals and supports the overall prevention of streptococcal infections within the household.
-
Health Monitoring and Follow-Up: After being diagnosed with strep throat, it is important to adhere to the prescribed antibiotic treatment and follow up with healthcare providers as needed. Monitoring symptoms, adhering to medication schedules, and seeking medical attention in the event of any complications are essential aspects of managing strep throat effectively. By actively participating in the recovery process, individuals can contribute to their own well-being and minimize the impact of the infection on their daily lives.
By incorporating these additional precautions into the management of strep throat, individuals can create a supportive environment that promotes recovery and minimizes the risk of bacterial transmission. These measures align with the principles of effective infection control and personal hygiene, contributing to the overall well-being of individuals and the maintenance of a healthy living environment.
Read more: When Should I Change Toothbrush After Covid
Conclusion
In conclusion, the management of strep throat extends beyond the administration of antibiotic treatment and encompasses various aspects of personal hygiene, household precautions, and proactive measures to prevent the spread of the bacteria. The potential contamination of toothbrushes with streptococcal bacteria highlights the importance of promptly changing toothbrushes after being diagnosed with strep throat. By adhering to the recommended time frame for replacing toothbrushes, individuals can significantly reduce the risk of reinfection and contribute to the overall containment of the bacteria within their living environment.
Furthermore, the understanding of strep throat as a contagious bacterial infection underscores the significance of implementing comprehensive precautions to minimize the risk of transmission. From practicing diligent hand hygiene to disinfecting common surfaces and separating personal items, these measures collectively contribute to creating a supportive environment that promotes recovery and prevents the spread of the bacteria to others.
The proactive approach to managing strep throat aligns with the principles of effective infection control and personal hygiene, emphasizing the importance of individual responsibility in safeguarding both personal well-being and the health of others. By integrating these precautions into daily routines and household management, individuals can actively contribute to the prevention of recurrent infections and support the overall well-being of their families and communities.
In essence, the management of strep throat extends beyond medical treatment and encompasses a holistic approach to infection control and preventive measures. By recognizing the potential risks associated with streptococcal bacteria and taking proactive steps to mitigate these risks, individuals can play a pivotal role in creating a safe and healthy living environment for themselves and those around them. Through informed decision-making and adherence to recommended guidelines, individuals can effectively navigate the challenges posed by strep throat and contribute to the overall containment of this contagious bacterial infection.
Frequently Asked Questions about When To Change Toothbrush After Strep
Was this page helpful?
At Storables.com, we guarantee accurate and reliable information. Our content, validated by Expert Board Contributors, is crafted following stringent Editorial Policies. We're committed to providing you with well-researched, expert-backed insights for all your informational needs.














0 thoughts on “When To Change Toothbrush After Strep”